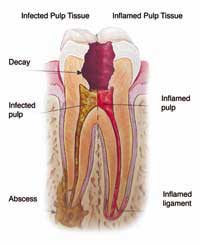
It doesn’t seem so long ago that dental implants appeared to be a threat to the future of specialist endodontic practice. Some 15 years ago, instead of being offered root canal treatment, patients with problematic molars were being offered a dental implant to replace the compromised tooth. A dental implant, so patients were told, operated just like a natural tooth. For not much more money, the filled and damaged molar which had caused the patient pain and discomfort could be replaced by an artificial tooth which offered a long-term solution. What was not to like?
It was to challenge this orthodoxy prevalent in the early part of this century, I spear-headed the Saving Teeth Awareness Campaign. My aim was to highlight that if the biological tooth can be saved, it should be. A dental implant can never be justified for a tooth which has not previously undergone root canal treatment and which is restorable.
A lot of colleagues felt the same way as I did and the campaign garnered considerable support. Not long after this, implant surgeon Michael Norton and myself undertook some public debates.
I would make the case for endodontics and he would make the case for dental implants. The key to the success of these presentations was the clinical consensus on the most critical issues. Instead of descending into an embarrassing disagreement, Michael and I could shake hands in the safe knowledge that we would both put the interests of patients first - if a tooth can be saved, it should be. We communicated the positive message that implants and endodontics can work in harmony to the benefit of patients. We argued that researchers should use the same criteria when studying the outcomes of both modalities. Implants tend to be measured according to their survival rate whereas endo studies measure the re-occurrence of disease.
The tables were already turning a little. Since then, they have turned even further. What were promised as long-term solutions for patients are failing in about 20% of patients. This is partly the result of emerging research in the field of periodontology – the specialist area dedicated to gums – which shows there is a worrying increase in peri-implantitis, a condition which can cause an implant to fail. A recent study shows that maintaining a periodontally compromised furcation involved molar is less costly than its extraction and replacement with an implant supported crown and is likely to be retained for a longer time period, irrespective of the degree of furcation involvement. For those of you who aren’t au fait with dental terminology, the furcation is where the roots divide; a furcation-involved molar suffers bone loss caused by periodontal disease. Treating disease in this hard-to-reach location is extremely challenging and needs the intervention of a gum specialist and the long-term support of a hygienist. Who could have predicted 20 years ago that we would be reappraising the dental implant so radically?
As we start 2016, hopefully everyone in the dental profession would agree that whilst dental implants are a good option for the right patient they may be ill-advised for patients with a history of periodontal disease. To quote the American endodontist and colleague Cliff Ruddle, the natural tooth is the ultimate dental implant.
Read More